Acute Pancreatitis
Acute Pancreatitis. Ashley Duckett, MD Theresa Cuoco, MD, FACP. Objectives. Identify clinical presentation and etiologies of acute pancreatitis Recognize the importance of severity of pancreatitis in determining management and outcomes
Share Presentation
Embed Code
Link
Download Presentation
- pancreatic
- organ failure
- pancreatic necrosis
- acute pancreatitis
- 30 pancreatic necrosis
- sod dysfunction pancreatic divisum

victoria-odonnell + Follow
Download Presentation
Acute Pancreatitis
An Image/Link below is provided (as is) to download presentation Download Policy: Content on the Website is provided to you AS IS for your information and personal use and may not be sold / licensed / shared on other websites without getting consent from its author. Content is provided to you AS IS for your information and personal use only. Download presentation by click this link. While downloading, if for some reason you are not able to download a presentation, the publisher may have deleted the file from their server. During download, if you can't get a presentation, the file might be deleted by the publisher.
Presentation Transcript
- Acute Pancreatitis Ashley Duckett, MD Theresa Cuoco, MD, FACP
- Objectives • Identify clinical presentation and etiologies of acute pancreatitis • Recognize the importance of severity of pancreatitis in determining management and outcomes • Understand the indications for imaging and antibiotics in acute pancreatitis
- Key Messages • Early aggressive hydration is critical in the management of acute pancreatitis. • Imaging with contrasted CT or MRI is indicated at 48-72 hours in patients with severe disease. • Early enteral nutrition improves outcomes in patients with severe pancreatitis. • Severity scores can be used to triage patients at risk for complications.
- Clinical presentation • Abdominal pain, distention • Nausea/vomiting (90%) • Fever, tachycardia, shock, coma • Dyspnea (pleural effusion) • Shallow respirations (diaphragmatic irritation) • Jaundice • Grey-Turner’s/Cullen’s 1% - intraabdominal hemorrhage
- Etiologies • Gallstones- 35-40% (increased ALT >150 is 50% sensitive and 96% specific) *women • Alcohol – 30% *men • Hypertriglyceridemia • Hypercalcemia • Post-ERCP -3% of diagnostic, 25% if SOD studies • Drugs – direct toxic, immunologic, ischemic causes – cocaine, HCTZ • Genetic mutations • Trauma • Infection – Viruses (mumps, hep B, CMV, HIV), Bacteria (mycoplasma, legionella, salmonella), fungi, parasites • Idiopathic -15-20% • Autoimmune (although usually presents mimicking neoplasm) • Scorpion bite • SOD dysfunction? Pancreatic divisum?
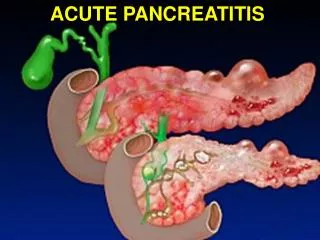
- Pathophysiology • Activation of trypsin in acinar cells • Activating multiple pancreatic digestive enzymes (synthesized but not secreted) • Leak into interstitial space and systemic circulation • Intrapancreatic Inflammation • Mediated by cytokines/inflammatory markers • SIRS • Extrapancreatic Inflammation • ARDS • Multiple organ failure (MOF) • Respiratory, cardiovascular, renal
- Diagnosis • Requires 2 of the following 3 features • Characteristic abdominal pain • Epigastric, band-like radiating to back, assoc n/v • Amylase and/or lipase >/= 3 times the upper limit • Amylase rises in 6-12 hrs, elevated 3-5 days • Lipase sensitivity 85-100%; more specific than amylase • Characteristic CECT (contrast enhanced CT) findings (or MRI/US) • Edema, peripancreatic fat stranding, necrosis, calcifications, pancreatic heterogeneity
- Imaging • Plain XR – unremarkable or have “sentinel loop” (localized ileus) or “colon cutoff sign” in severe disease • CXR – pleural effusion suggests increased risk of complications • Abd ultrasound: diffuse, hypoechoic pancreas, useful for gallstones, not good for necrosis • CT scan – useful for complications and for severity assessment • When to CT? indicated if need to assess for necrosis (severe disease) at 48-72 hours • Oral and IV contrast preferred (to diagnose necrosis, calcifications, stones, mass) • MRCP – best for delineating fluid collections, necrosis, ducts, looking for choledocholithiasis
- Management • Determine etiology – history, LFTs, TGs, calcium, abdominal ultrasound for stones • Determine severity and send severe to ICU • FLUIDS FLUIDSFLUIDS – Initial bolus, then 250-300cc/hr x 48 hours if cardiac fx normal • Increasing BUN at 24 hrs predicts mortality • Monitor glucose and lytes (Ca, Mg) • No daily amylase/lipase; no correlation with severity • Pain management • Nutrition – start oral feeds when pain improving, no ileus in mild dz
- Nutrition • Need for nutrition and pancreatic rest in severe pancreatitis or anyone NPO > 5 days • Early enteral nutrition (at 24-48 hrs) reduces mortality, multi-system organ failure, infections and need for operative interventions compared to TPN • Maintains intestinal barrier, prevents translocation • High protein, low fat formula
- Antibiotics • ACG – prophylactic antibiotics not recommended • AGA – abx should be restricted to pts with >30% pancreatic necrosis by CT and should be used for less than 14 days • Meropenem or imipenem are drugs of choice • CT guided aspiration/culture recommended if infected pancreatic necrosis is suspected (fevers, sepsis, increasing WBC)
- Classification of Acute Pancreatitis • Interstitial edematous • Acute inflammation of pancreatic parenchyma and peripancreatic tissue • Necrotizing Acute Pancreatitis • 5-10% of patients • Pancreatic or peripancreatic necrosis • Appears as non-enhancing area • Early CECT may underestimate (wait 48-72h)
- Severity of Pancreatitis • Mild Acute • No organ failure, local or systemic complications • Moderately Severe • Transient organ failure (OF) 48h) • Mortality ~36-50%; higher w infected necrosis
- Severity scores • Most cases mild, 15-25% severe • Depends on presence and duration of organ failure • Early risk stratification (median time to ICU transfer is 24 hours after admission) • APACHE II most widely used – score >8=severe • BISAP – simple, can be done early • BUN, AMS, SIRS, Age>60, pleural effusion • >3 points indicates increased risk of death • Ranson’s criteria
- Ranson’s Criteria At admission At 48 hrs out Ca < 8 HCT fall >10% PO2 < 60 BUN increase >5 Base deficit > 4 mEq/L Sequestration of fluids > 6L • Age > 55 • WBC > 16 • Glu > 200 • AST > 250 • LDH > 350
- Complications • Pancreatic necrosis – becomes infected in about 30%; usually monomicrobial (Ecoli, Pseudomonas, Kleb) • Abscesses • Pseudocysts -Drainage prior to maturation (6 wks) can lead to complications • Splenic vein thrombosis (up to 19% of pts) • Anticoagulation may be needed for complications • Abdominal compartment syndrome • ARDS, shock, renal failure, GI bleeding
- Definitions of Pancreatic and Peripancreatic Fluid Collections • APFC: Acute Peripancreatic Fluid Collection • Assoc w intersitialpanc; no necrosis • Homogenous; no definable wall; adjac to pancreas • Pancreatic Pseudocyst • Well circumscribed, homogenous, with wall • Maturation usually >4 weeks after acute panc • ANC: Acute Necrotic Collection • Only in setting of necrotizing panc • Heterogenous, no wall, intra and/or extra pancreatic • WON: Walled Off Necrosis • Heterogenous, well defined wall, intra/extra • Maturation >4 weeks after acute necrotizing panc
- Gallstone pancreatitis – early ERCP or surgery? • Early ERCP or surgery to remove bile duct stones may decrease severity of pancreatitis • ERCP within 72 hours in pts with cholangitis OR concern for stone (stone on imaging, dilated CBD, jaundice, rising LFTs) • All patients with gallstone panc should have cholecystectomy • 25-30% risk of recurrent panc, cholecystitis or cholangitis in
- References • Banks P et al. Practice Guidelines in Acute Pancreatitis. Am J Gastroenterol 2006; 101:2379-2400 • Banks P et al. Classification of acute pancreatitis-2012:revision of the Atlanta classification and definitions by international consensus. Gut 2013; 62: 102-111. • Al-Omran M et al. Enteral versus Parenteral Nutrition for Acute Pancreatitis (Review). Cochrane Database of Systematic Reviews 2010, Issue1 • Falor et al. Early Laparoscopic Cholecystectomy for Mild Gallstone Pancreatitis. Arch Surg 147: Nov 2012 • Van Santvoort et al. Early Endoscopic Retrograde Cholangiopancreatography in Predicted Severe Acute Biliary Pancreatitis: A Prospective Multicenter Study. Annals of Surgery. 250 (1); July 2009 • Wu, Bechien. Prognosis in Acute Pancreatitis. CMAJ: 183 (6); April 2011
Acute Pancreatitis
Acute Pancreatitis. Acute Pancreatitis - Objectives. Discuss basic physiology Etiology Clinical Presentation Diagnosis Prognosis Management Complications. Pancreatic Physiology.
1.73k views • 39 slides
Acute Pancreatitis
Acute Pancreatitis. Prof. Yousri Taher Head Of HPB Unit Alexandria University. Acute Pancreatitis. Is a discrete episodes of inflammation resulting from intrapancreatic activation of digestive enzymes. It is a disease of wide spectrum of severity complications and outcome.
1.63k views • 38 slides
Acute Pancreatitis
J.H.. JH is a 64-yr-old male admitted to an outside hospital with a 4 day history of progressively worsening epigastric pain without radiation. . History. What other points of the history do you want to know?. History, J.H.. Characterization of symptomsTemporal sequenceAlleviating / Exacerbating
1.67k views • 60 slides
ACUTE PANCREATITIS
GROUP D Mamba-Medinilla. ACUTE PANCREATITIS. Etiologies of Acute Pancreatitis. Common Causes. Uncommon Causes. Vascular causes CT disorders Cancer of the pancreas Hypercalcemia Periampullary diverticulum Pancreas divisum Hereditary pancreatitis Cystic Fibrosis Renal Failure.
937 views • 37 slides
Acute Pancreatitis
Acute Pancreatitis. Dr. Belal M. Hijji, PhD, RN April 2 & 4, 2011. Learning outcomes. By the end of this lecture, students will: Have an introductory statement about acute pancreatitis. Identify clinical manifestations. Describe diagnostic evaluation.
428 views • 18 slides
Acute pancreatitis
Acute pancreatitis. Introduction . Acute pancreatitis is the acute inflammation of the pancreas and is characterized by: by upper abdominal pain , vomiting , fever , tachycardia , elevated WBC, and elevated serum amylase. Etiology .
4.49k views • 8 slides

Introduction – acute pancreatitis
Early ERCP and biliary sphincterotomy with or without small caliber pancreatic stent in patients with gallstone pancreatitis (nonrandomized, prospective, dual center trial). Z.Dubravcsik 1 , A.Szepes 1 , R.Fejes 2 , G.Balogh 2 , Z.Virányi 1 , P.Hausinger 1 , A.Székely 2 , L.Madácsy 2
491 views • 18 slides
Acute pancreatitis
Acute pancreatitis. Dr.Alaa Mohammed Fouad Mousli Surgical Demonstrator. Acute pancreatitis. INTRODUCTION :
859 views • 15 slides
Acute Pancreatitis
Acute Pancreatitis. Steven B. Goldin, MD University of South Florida. J.H. JH is a 64-yr-old male admitted to an outside hospital with a 4 day history of progressively worsening epigastric pain without radiation. History. What other points of the history do you want to know?.
1.34k views • 60 slides
Acute Pancreatitis
Acute Pancreatitis. Presented by: Ahmad Pourhosseini. BODY. common bile duct. TAIL. HEAD. pancreatic duct. ampulla. UNCINATE. pancreatic enzymes. Digestive Enzymes in the Pancreatic Acinar Cell. PROTEOLYTIC LIPOLYTIC ENZYMES ENZYMES Lipase Trypsinogen Prophospholipase A2
811 views • 36 slides
Acute Pancreatitis
Acute Pancreatitis. Resident Conference October 5, 2004 Rachel Dunagin, MD. Background. Acute Inflammatory process of pancreatic parenchyma A stimulus leads to release of activated digestive enzymes from acinar cells into interstitium Results in autodigestion of pancreas and adjacent tissue
1.36k views • 64 slides
Acute Pancreatitis
Acute Pancreatitis. Umit Akyuz , MD Gastroenterology Department,Yeditepe University Istanbul. Acute Pancreatitis - Objectives. Discuss basic physiology Etiology Clinical Presentation Diagnosis Prognosis Management Complications. Pancreatic Physiology.
1.96k views • 68 slides
ACUTE PANCREATITIS
ACUTE PANCREATITIS. By: Maj.Gen.Badshah khan Prof. & HOD Medicine YMDC. INTRODUCTION. Pancreatitis is divided into acute and chronic.
2.27k views • 20 slides

ACUTE PANCREATITIS
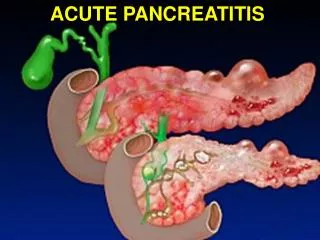
ACUTE PANCREATITIS. ANATOMY. ACUTE PANCREATITIS. -Acute pancreatitis (AP) are characterized by edematous lesions, eventually necrosis and bleeding inside and in peripancreatic area. Pathology: - 2 types of AP 1. Edematous AP congestion and edema of the pancreas . swelling
763 views • 32 slides
ACUTE PANCREATITIS
ACUTE PANCREATITIS. Surgical Anatomy. Surgical Anatomy. Although alcohol is the most common etiology of acute pancreatitis in developed countries. PAIN IRRADIATION ON ACUTE PANCREATITIS. METHODS OF EXAMINATION OF ACUTE PANCREATITIS. normal pancreatic duct. ERCP.
1.67k views • 48 slides
Acute Pancreatitis
Acute Pancreatitis. John Lieb II MD Assistant Professor of Clinical Medicine Division of Gastroenterology. “Acute Pancreatitis is the most terrible of all the calamities that occur in connection with the abdominal viscera.”. Sir Berkeley Moynihan Ann Surg 1925. Outline. Def
2.55k views • 78 slides
Acute pancreatitis
Acute pancreatitis. Acute Pancreatitis. Common condition Incidence 10-20/1000,000 population Mortality 5-10% 80% due to gallstones and alcohol. Drugs Azathioprine Furosemide Tetracycline Methyldopa . Trauma Viral Infection Hypercalcaemia Hyperlipidaemia Scorpion Bite!. Other Causes.
976 views • 35 slides
Acute Pancreatitis
Acute Pancreatitis. Steven B. Goldin, MD University of South Florida. J.H. JH is a 64-yr-old male admitted to an outside hospital with a 4 day history of progressively worsening epigastric pain without radiation. History. What other points of the history do you want to know?.
961 views • 60 slides
Acute pancreatitis
Acute pancreatitis. The treatment of patients is dependent on the early assessment of disease severity. Potentially lethal attacks are known to occur in 2%–10% of patients with acute pancreatitis Early detect !. Classification. 1992 Atlanta, International Symposium on Acute Pancreatitis
787 views • 35 slides